Have you ever felt a strange, sharp discomfort in your lower abdomen and wondered why it appeared suddenly during an otherwise normal day? Many people discover diverticulitis this way because the early signs often hide behind familiar digestive sensations. According to our editor’s research, most individuals mistake the first symptoms for simple bloating or temporary cramps until the discomfort becomes more persistent. This moment of confusion usually leads people to seek clarity about what the condition truly means. Understanding these early signals makes the experience feel less overwhelming. Awareness supports calmer decisions and smoother care.
What is diverticulitis and why does it occur?
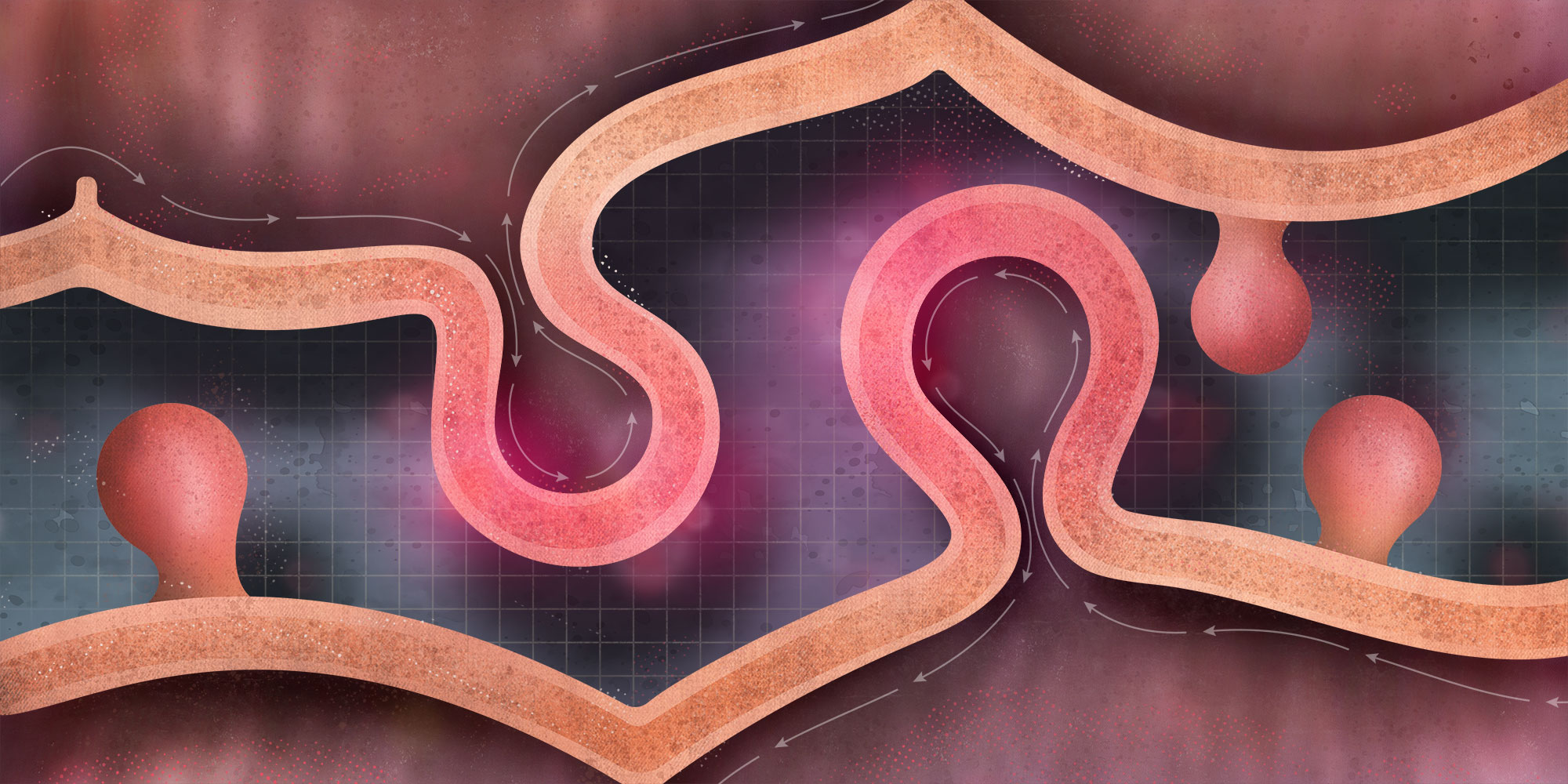
Diverticulitis develops when small pouches in the colon become inflamed. According to our editor’s reviews, these pouches, called diverticula, form naturally as the intestine ages. Many people live with diverticula without symptoms. The issue begins when one of them becomes irritated or infected. This irritation causes sharp pain and discomfort. People often feel the pain on the lower left side. Age, diet and lifestyle contribute to risk.
Why do some individuals develop inflammation?
Inflammation occurs when a pouch becomes blocked. According to our editor’s research, trapped material irritates the tissue. Bacteria grow inside the pouch. This growth triggers swelling and pain. People notice discomfort during movement or pressure. The inflammation spreads into surrounding tissue. This process explains the sudden intensity. Understanding this pattern provides clarity.
What early signs suggest diverticulitis?
Early signs involve steady pain and tenderness. According to our editor’s reviews, the discomfort grows stronger over hours rather than minutes. People often experience mild fever. Nausea becomes possible. Bowel habits may shift slightly. These signs mimic other digestive issues. Recognizing the combination helps identify diverticulitis early. Awareness supports timely care.
How does the body react during inflammation?
The body reacts with protective responses. According to our editor’s research, the intestine slows movement to reduce irritation. Pressure builds in the area. The immune system increases activity. This response creates heat, swelling and redness internally. People feel fatigued during this process. Appetite decreases naturally. These reactions reflect the body’s attempt to heal.
Why do some people confuse symptoms with other issues?
Symptoms overlap with common digestive conditions. According to our editor’s reviews, people often think they have simple constipation or gas. Pain patterns feel familiar. Early fever feels mild. Discomfort spreads gradually. These similarities cause confusion. Understanding diverticulitis reduces misinterpretation. Knowledge supports confidence.
How is diverticulitis diagnosed?
Diagnosis involves clinical evaluation. According to our editor’s research, doctors assess pain location and severity. Blood tests reveal inflammation levels. Imaging helps confirm affected pouches. These steps clarify the condition accurately. Diagnosis guides treatment decisions. Clear evaluation supports efficient care. Patients feel reassured.
Why is early diagnosis important?
Early diagnosis prevents complications. According to our editor’s reviews, untreated inflammation may worsen. Abscess formation becomes possible. Tissue damage increases risk. Early action prevents escalation. People recover faster with timely support. Awareness shortens discomfort. Early clarity protects long-term health.
What treatment options exist for mild cases?
Mild cases respond well to conservative care. According to our editor’s research, rest supports healing. Simple diet adjustments reduce strain. Hydration helps stabilize digestion. Short-term medication controls inflammation. People improve within days. Mild cases rarely require hospitalization. Gentle habits encourage smoother recovery.
Why does diet play a role during healing?
Diet affects inflammation response. According to our editor’s reviews, early healing requires low-fiber meals. This reduces stress on the colon. People gradually return to normal foods. Balanced choices prevent recurrence. Hydration supports smoother digestion. Diet becomes a practical tool. Awareness shapes improvement.
What foods support recovery?
Gentle foods reduce irritation. According to our editor’s research, broth, yogurt and soft grains help calm symptoms. These options allow easier digestion. People feel less discomfort during meals. Once healed, fiber-rich foods help prevent future issues. Balance protects the colon. Healthy habits strengthen resilience.
Why does fiber help prevent future episodes?
Fiber improves stool movement. According to our editor’s reviews, this prevents pouch blockage. Fiber softens stool naturally. The colon experiences less pressure. People feel more regular. This reduces inflammation risk. Fiber becomes essential after healing. Balanced intake supports long-term stability.
How do antibiotics help treat diverticulitis?
Antibiotics target bacterial growth. According to our editor’s research, inflammation often involves infection. Medication reduces bacteria quickly. Pain improves over days. Fever decreases with treatment. People feel stronger gradually. Antibiotics support safe healing. Follow-up ensures proper response.
Why do some cases require stronger intervention?
Some cases become more severe. According to our editor’s reviews, complications like abscess or rupture require advanced care. These situations demand hospitalization. Intravenous therapy stabilizes inflammation. Surgery may become necessary. Intense cases need structured support. Early care reduces severity risk.
What happens when an abscess forms?
An abscess develops when infection becomes trapped. According to our editor’s research, fluid collects inside the pouch. This creates pronounced swelling. Pain intensifies noticeably. Drainage becomes necessary for relief. Treatment prevents further spread. Abscess care protects surrounding tissue. Healing continues with monitoring.
How does surgery help complicated cases?
Surgery removes damaged sections. According to our editor’s reviews, this prevents future inflammation. Procedure choice depends on severity. Some individuals need temporary support bags. Others heal without additional devices. Surgery restores function safely. Postoperative care ensures stability. Surgical decisions rely on careful evaluation.
Why do some individuals experience recurring episodes?
Recurrence happens when risk factors remain. According to our editor’s research, low fiber intake increases risk. Dehydration affects stool movement. Sedentary habits slow digestion. Stress influences intestinal rhythm. People with persistent habits face more episodes. Adjustments prevent recurrence. Awareness guides prevention.
How do lifestyle changes reduce risk?
Lifestyle changes support colon health. According to our editor’s reviews, gentle movement improves bowel rhythm. Hydration enhances digestion. Balanced meals prevent blockage. Stress reduction stabilizes intestinal patterns. These habits protect the colon daily. Consistency strengthens resilience. Change grows gradually.
Why does hydration matter so much?
Hydration maintains stool softness. According to our editor’s research, dry stool increases pressure. This pressure irritates diverticula. Water supports colon function. Hydration reduces pain risk. People feel more comfortable daily. Proper intake prevents issues. Water becomes essential.
How does stress influence diverticulitis risk?
Stress affects digestive movement. According to our editor’s reviews, tension slows intestinal rhythm. Slower movement increases pressure. This pressure complicates diverticula health. Stress also influences inflammation levels. People feel symptoms during intense weeks. Managing stress supports stability. Calm routines protect the colon.
What long-term habits support colon strength?
Long-term habits maintain stability. According to our editor’s research, fiber intake supports healthy movement. Hydration prevents blockage. Gentle exercise enhances rhythm. Balanced meals reduce pressure. These habits guide healthier patterns. Daily choices shape colon resilience. Consistency creates comfort.
Where should individuals begin after diagnosis?
Beginning starts with clear understanding. According to our editor’s reviews, people benefit from learning symptoms and triggers. Gentle diet adjustments support healing. Routine hydration helps quickly. Stress awareness influences comfort. These early steps create smoother recovery. Confidence grows with knowledge.
