Have you ever eaten a meal and felt more than simple heaviness afterward, a deep upper abdominal pain that spreads toward your back and refuses to settle. Many people first hear the word pancreatitis in an emergency department or after a worrying scan. It sounds serious, and in many cases, it is. According to our editor’s research, pancreatitis means the pancreas is inflamed and not working as it should. That inflammation affects how your body handles food, especially fats and proteins. To see why, it helps to understand what this quiet organ and its digestive enzymes normally do for you every single day.
What the pancreas actually does in digestion
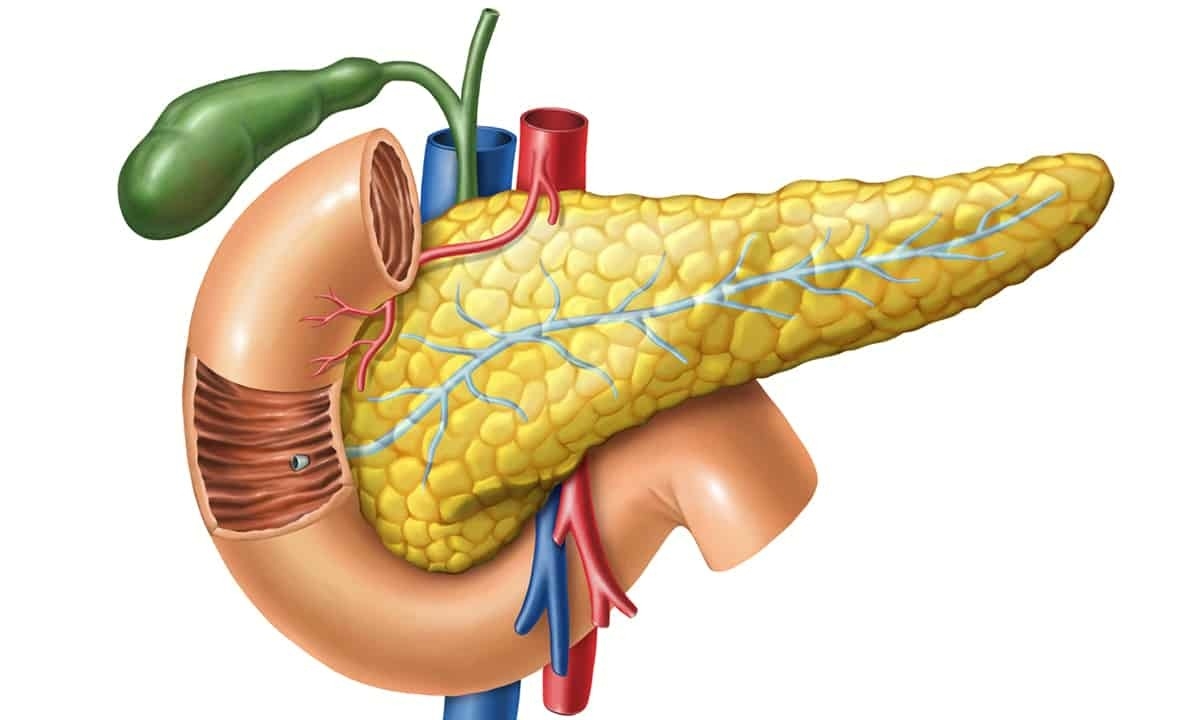
The pancreas sits behind your stomach, tucked deep in the upper abdomen. It has two main roles, one related to digestion and one related to blood sugar. On the digestive side, it produces enzymes that break down fats, proteins, and carbohydrates. These enzymes travel through small ducts into the small intestine when you eat. Lipase helps digest fats, amylase helps with starches, and proteases help with proteins. According to our editor’s research, this enzyme mix allows nutrients to be absorbed efficiently further along the gut. When the pancreas works smoothly, you rarely think about it. When it goes wrong, digestion can change dramatically.
What happens in pancreatitis
Pancreatitis simply means inflammation of the pancreas, but that word hides complex processes. In healthy digestion, enzymes activate in the intestine, not inside the pancreas. In pancreatitis, those enzymes can activate too early and start irritating pancreatic tissue. The organ swells, becomes painful, and its function drops. Acute pancreatitis develops suddenly, often with strong pain and vomiting. Chronic pancreatitis develops more slowly, with ongoing damage and scarring over time. According to our editor’s research, both forms affect digestion, but chronic cases usually cause longer term enzyme problems. The more the tissue is damaged, the fewer enzymes reach your intestine.
Common causes and risk factors
Several triggers appear again and again in medical reports on pancreatitis. Gallstones can block the duct that drains digestive juices from the pancreas. Alcohol, especially heavy or long term use, is a frequent factor in many countries. Certain medicines, high triglycerides, and abdominal injuries also appear as causes. Sometimes, no clear cause is found, which frustrates patients and doctors alike. Chronic pancreatitis often connects to repeated acute attacks, long term alcohol use, or genetic conditions. According to our editor’s research, gallstones and alcohol remain the most widely reported contributors worldwide. Knowing these patterns helps doctors choose tests and guide lifestyle advice.
Typical symptoms you might notice
The most famous symptom is upper abdominal pain, often central or slightly left sided. It may feel deep, burning, or gripping, and can spread into the back. Many people find it worsens after eating, especially after fatty meals. Nausea and vomiting often join, and appetite drops quickly. In more severe cases, there may be fever, rapid pulse, or a very unwell feeling. Chronic pancreatitis can bring milder but persistent pain, unintended weight loss, and greasy, pale, foul smelling stools. According to our editor’s research, these oily stools signal poor fat digestion due to low enzyme output. Any sudden severe pain of this kind needs urgent medical assessment, not home guessing.
How doctors usually diagnose pancreatitis
Diagnosis blends symptoms, blood tests, and imaging. Blood tests often measure amylase and lipase, the digestive enzymes that leak into the bloodstream during inflammation. Elevated levels support the diagnosis, especially in acute attacks. Ultrasound or other scans help look for gallstones, swelling, and duct problems. In chronic cases, imaging might show calcifications or scarring in the pancreas. Doctors also ask about alcohol intake, medicines, and previous abdominal problems. According to our editor’s research, guidelines stress the importance of ruling out other emergencies like heart issues or ulcers. Pancreatitis is one possibility among several when upper abdominal pain appears suddenly.
Why pancreatitis affects digestive enzymes
When the pancreas becomes inflamed, enzyme production and delivery can drop. Imagine a factory where several machines break down and the main exit becomes blocked. Even if some enzymes are produced, they may not reach the intestine effectively. In mild acute cases, this disruption may be temporary and improve with healing. In chronic pancreatitis, repeated damage gradually destroys enzyme producing cells. As a result of our editor’s reviews, many chronic patients develop pancreatic exocrine insufficiency. That term simply means the pancreas can no longer produce enough digestive enzymes for normal food breakdown. Without support, this leads to malabsorption and nutritional problems.
Signs that enzyme production might be low
Low digestive enzyme output does not always scream for attention at first. People notice bloating, gas, and discomfort after meals, especially with fatty foods. Stools may become bulky, pale, greasy, and harder to flush. Weight can drop despite normal or even increased eating. Fat soluble vitamin levels, such as vitamin D and vitamin A, may fall over time. Some patients feel unusually tired or notice thinning hair and brittle nails. According to our editor’s research, these symptoms often appear gradually in chronic pancreatitis. They hint that food is passing through without being fully digested and absorbed.
Pancreatic enzyme replacement therapy in simple terms
When the pancreas does not supply enough enzymes, doctors may prescribe pancreatic enzyme replacement therapy. These are capsules containing a mixture of digestive enzymes designed to mimic natural pancreatic juice. People usually take them with meals and snacks to help break down food. The dose depends on weight, meal size, and symptom response. If the dose is too low, greasy stools and bloating may continue. If used correctly, many patients report less discomfort and improved weight stability. According to our editor’s research, enzyme replacement does not cure pancreatitis, but it can strongly improve quality of life. It supports digestion while doctors address underlying causes and pain.
How to use prescribed enzymes effectively
Using enzymes well requires attention to timing and consistency. They usually need to be taken at the start of a meal, sometimes spread across the meal. Swallowing the whole capsule allows tiny coated particles to mix with food in the gut. Chewing capsules or crushing them can damage that protective coating and reduce effectiveness. Doctors often adjust doses based on stool changes and weight trends. As a result of our editor’s reviews, patient education is key for good results. When people understand how these medicines work, they are more likely to take them properly with food.
The role of diet in pancreatitis management
Diet choices matter, but they depend on the phase and severity of pancreatitis. In acute attacks, doctors may limit eating initially to let the pancreas rest. Once stable, patients often move toward small, frequent, low fat meals. In chronic pancreatitis, a balanced diet still matters, but large fatty meals may worsen symptoms. Some people benefit from tailoring fat intake while using enzyme replacement. Alcohol avoidance is usually strongly advised, as it can provoke further attacks. According to our editor’s research, dietitians familiar with pancreatic disease provide valuable, personalised guidance. They help balance nutritional needs with symptom control and real life preferences.
Why self treating with supplements can be risky
Digestive enzyme supplements are widely sold, which can tempt people with unexplained symptoms to self medicate. However, not all supplements match the potency or content of prescription products. Some do not survive stomach acid or provide the necessary mix of enzymes. More importantly, using them without proper diagnosis might mask serious conditions. Pancreatitis, coeliac disease, gallbladder problems, or cancers can all affect digestion. According to our editor’s research, health authorities regularly caution against replacing medical evaluation with random supplements. Any ongoing pain, weight loss, or greasy stools deserves proper assessment rather than guessing.
Possible complications doctors watch for
Pancreatitis is not only about pain and digestion, it can affect other systems too. Severe acute pancreatitis may cause dehydration, low blood pressure, or breathing problems. Fluid collections or cyst like spaces can form around the pancreas. Infections and organ failure are serious, hospital level complications requiring close monitoring. Chronic pancreatitis can increase the risk of diabetes as insulin producing cells are damaged. Bone health can suffer if vitamin D and calcium absorption stay low. According to our editor’s research, regular follow up helps detect these issues earlier. Long term care focuses not just on the pancreas, but on overall health stability.
Living with chronic pancreatitis day to day
Living with chronic pancreatitis often means adjusting routines, not giving up on life. Pain management, enzyme therapy, and careful diet all play parts. Some people track trigger foods and times of day when symptoms flare. Others learn pacing strategies for energy, balancing activity with rest. Psychological support or peer groups can help with frustration and fear. As a result of our editor’s reviews, people cope better when they understand their condition. Clear explanations reduce the mystery and help them recognise when something feels different or worrying. Education turns a frightening diagnosis into a condition that can be monitored and managed.
When to seek urgent medical attention
Certain signs should always prompt quick medical help rather than watchful waiting. Sudden, severe abdominal pain that will not ease needs prompt assessment. Pain spreading to the back, especially with vomiting or fever, deserves attention. Yellowing of the skin or eyes, known as jaundice, can signal bile duct issues. Rapid heart rate, shortness of breath, or feeling faint are also concerning features. According to our editor’s research, early treatment in acute pancreatitis improves outcomes. It allows doctors to manage fluids, pain, and complications more effectively from the start. Do not delay because you hope the pain will simply settle by morning.
How to talk with your healthcare team about enzymes
If you have pancreatitis or suspect enzyme issues, clear questions help. You might ask whether your symptoms suggest pancreatic exocrine insufficiency. You can ask if enzyme replacement is appropriate and how dosing works. It is reasonable to ask what stool changes to watch for and when to adjust treatment. Bringing a simple symptom diary can make these conversations more focused. According to our editor’s research, people who understand their enzyme plan feel more confident eating. They worry less about every meal and can enjoy food while respecting medical advice. That balance supports both physical health and emotional wellbeing.
